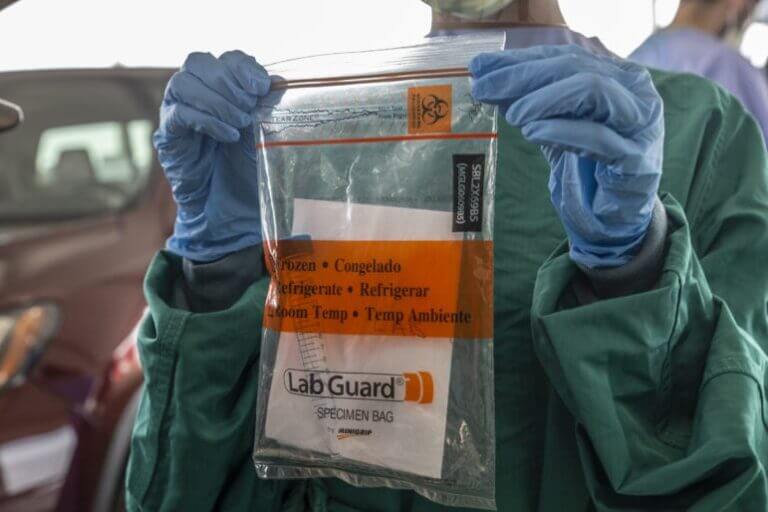

Eric J. Shelton/Mississippi Today, Report For America
The materials used to collect and contain the specimen from those potentially infected with COVID-19 is shown in a a mock COVID-19 specimen collection at the Mississippi State Fairgrounds in Jackson, Miss., Monday, March 23, 2020.
Mississippi has the most COVID-19 cases per capita among nursing home residents in the U.S. As cases surge across the state, nearing peak levels seen over the summer, outbreaks in long-term care facilities have increased by nearly 25% over the last week alone.
Currently, 140 facilities have outbreaks — defined as a single case among residents and two or more cases among staff over the last two weeks — up from 113 a week ago, comprising 147 more cases and 22 deaths in one week’s time. With only 211 facilities in the state, over two-thirds currently have active cases.
Nationally, Mississippi has the most cumulative cases per 1,000 residents since the pandemic began, at 407 per capita, according to data collected by the Centers for Medicare and Medicaid that regulates nursing homes. Other southern states follow closely: Alabama (404), Arkansas (395) and South Carolina (392).
Too, Mississippi has the fifth highest death rate among nursing homes, with 83 residents dying from COVID-19 out of every 1,000. New Jersey has the most at 120 deaths per capita.
Overall, almost half of all long-term care residents have contracted the coronavirus — 7,131 cases out of just over 16,000 total residents — and 20% of those who contract the virus in a nursing home die.
In September, the Mississippi State Department of Health stopped reporting nursing home outbreaks by facility and began relying on Medicare data to track nursing home outbreaks. In June, the state health department began listing facility names after a court order.
The state cited duplicate reporting as the reason for the switch to relying on Medicare facility data, but still tracks active and cumulative outbreaks by county.
But some nursing homes aren’t reliably submitting their data to Medicare.
As of Thursday’s nationwide reporting, 10 Mississippi nursing homes didn’t submit data at all. Of the 194 who did submit data, Medicare flagged nine as not passing “quality assurance,” meaning their data could be unreliable due to incorrect reporting.
Including those who don’t report or do so incorrectly, nearly 10% of Mississippi’s nursing home COVID-19 data is unreliable, so the true rate of cases among residents is unknown.
Two 60-bed facilities in the Pine Belt — which saw early broad community spread, but has flattened virus spread over time — have seen the highest rate of nursing home cases in the state. Due to a high rate of deaths, both facilities have had more cases than they currently have residents — both currently have 39 residents.
Laurelwood Community Living Center has seen the most cases per capita across the pandemic, at 1,846 cases per 1,000 residents, or an 185% infection rate. The proportion of cases is larger than 100% because more people have contracted the virus and died from it than the total number of current residents.
Of those who contract the virus in the Laurel facility, 40% have died. In total 72 residents and 17 staff members have tested positive for the virus, and 38 have died.
Leakesville Rehabilitation and Nursing Center in Greene County has had 59 total cases among residents and 39 staff cases, comprising 1,512 cases for every 1,000 residents and a death rate of 29%. Both the Greene and Jones County facilities report conducting asymptomatic tests for staff and residents as a way of checking facility-wide exposure, which could inflate numbers by catching more asymptomatic cases.
The facilities are two of 12 in Mississippi that have had a cumulative infection rate of more than 100%, meaning their case total is more than their current resident census due to residents leaving the facility or dying.
Neither facility reported new cases to Medicare since November. The Laurel facility said through a spokesperson that the nursing home is currently “COVID free” and provided the following statement: “Taking care of people in their time of need is what we do. Since the very beginning of COVID this is what we have planned for and are meeting the challenge. Once a COVID “outbreak” occurs we put in controlled checkpoints for all employee shifts and visitors are maintained. Then we have isolation areas for the patient along with any additional cases that may ensue. Team member (sic) that are positive are sent home to quarantine and follow the CDC guidelines. Our team has a COVID plan in working closely with our suppliers and state and local agencies to maintain sufficient PPE, supplies, and equipment.”
The Leaksville facility did not respond to request for comment.
Of the ten Mississippi facilities with the most cases per capita, seven are for-profit owned and all have been cited for deficiencies by Medicare — eight for improper infection control before the pandemic began, according to nursing home inspection data. For-profit nursing homes have had twice as many COVID-19 cases and three times the deaths compared to government or non-profit facilities, according to analysis by the Mississippi Center for Investigative Reporting.
Many Mississippi nursing homes report resource shortages, but notably not when it comes to testing. Just five nursing homes reported being unable to adequately test residents. Even so, fewer than a quarter of facilities reported testing all staff and residents after a new case, despite the Centers for Disease Control and Prevention recommending such testing.
Just 80 facilities, a little over a third, test residents without exposure, known as surveillance testing — widely regarded as the most effective way to judge actual case burden and isolate spread. In May, the state health department tested all nursing home staff and residents, successfully thwarting off worsening spread among facilities at the time.
Afterward though, many facilities started to open back up as outbreaks remained relatively stable over early summer. But as community spread worsened over the summer, nursing home cases followed suit. By late July when the state saw it’s daily case peak, 95% of the state’s facilities had concurrent outbreaks.
Despite the growing cases and efficacy of surveillance testing, only two-thirds of facilities test asymptomatic staff for surveillance of disease spread.
A quarter of nursing homes reported shortages in nurses and 10% don’t have a week’s worth of N-95 masks, the gold standard for medical use. Both shortages point to long-standing resource strains that hamper nursing home’s ability to fight the virus in their facilities.
More than half of nursing homes across the nation are currently losing money, according to the American Health Care Association. The national lobbying group for nursing homes has ebbed and flowed in their messaging on the issue, changing their tone from stark cries for help early on to over the summer focusing on steps to safely re-open facilities to visitors over the summer.
Now, the group says widespread community spread — particular across the South and Midwest — is driving nursing homes into a third wave of infections. Nursing homes are asking to be among first-priority for COVID-19 vaccinations when they’re available — something Mississippi says it will accommodate, after front-line healthcare workers. CVS and Walgreens will partner with facilities for distribution, but further details have not yet been released.
The post Mississippi tops nation’s COVID-19 cases in nursing homes, where half of all residents have contracted the virus appeared first on Mississippi Today.
- UMMC keeps clinics closed and cancels elective procedures Monday and Tuesday amid recovery from cyberattack - February 22, 2026
- With school choice, what about the students left behind? - February 22, 2026
- Scott Colom raised most money, but Cindy Hyde-Smith has most cash before March primary - February 21, 2026