Violent Trump supporters break through a police barrier outside the U.S. Capitol on Wednesday. (AP Photo/Julio Cortez)
A mob of violent supporters of President Donald Trump stormed the U.S. Capitol on Wednesday as Congress counted the electoral votes to confirm President-elect Joe Biden’s presidential victory.
The pro-Trump rioters — incited earlier Wednesday morning by the president’s oldest son and other close allies of the president — assaulted Capitol Police officers, smashed windows and tore down security barricades on their way into the building, prompting officials to lock down both legislative chambers of the building and nearby congressional office buildings.
Several high-profile members of Congress were evacuated, and others were told to shelter in place during the lockdown. The electoral vote counting process was halted.
The mob — many of whom were visibly armed and carrying pro-Trump and Confederate flags — breached the Senate chamber, and others tried to break into the House chamber. Inside the House chamber, police officers drew guns to deter them from entering. Multiple news reports said at least one person was shot, and that authorities had found an improvised explosive device on the Capitol grounds.
Several rioters were placed in handcuffs and arrested as armored police worked to clear the building.
Staffers for all six delegates — Sen. Roger Wicker, Sen. Cindy Hyde-Smith, Rep. Trent Kelly, Rep. Bennie Thompson, Rep. Michael Guest and Rep. Steven Palazzo — said the members and their staffs are safe.
In a video posted to his Twitter account shortly after 3 p.m., Trump again used disproven rhetoric that “the election was stolen” and spoke in sympathetic and affectionate terms to the rioters, telling them to “go home.”
“I know you’re in pain. I know you’re hurt,” Trump said in the video. “…We love you. You’re very special.”
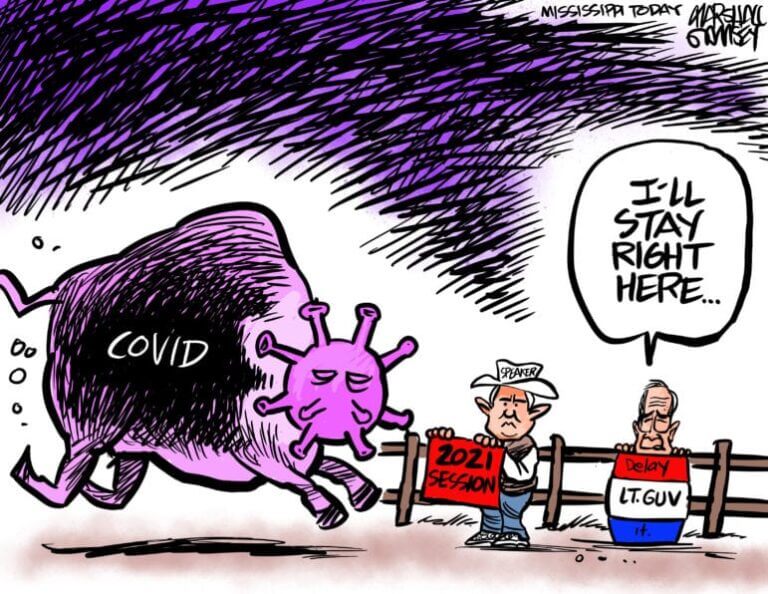
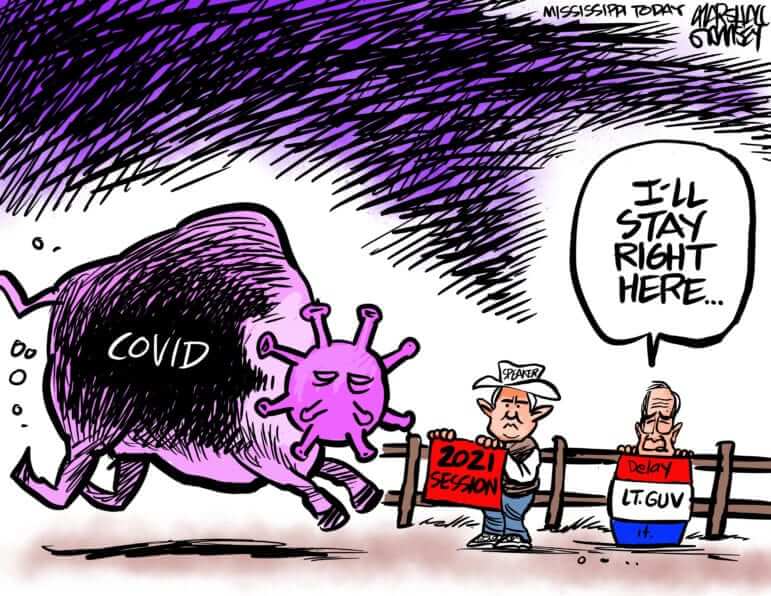
The chaos occurred in the nation’s Capitol on the same day the Mississippi Legislature took the final vote on adopting a new flag to replace the old banner that contained the Confederate battle emblem in its design.
People outside of the Mississippi Capitol, waving Trump banners and the old flag, protested peacefully throughout the much of the day.
As the assault was occurring in Washington, the Mississippi House was in session and many members did not know what was occurring.
Republican House Speaker Philip Gunn was informed of the events in Washington by a reporter and immediately began inquiring on what was occurring.
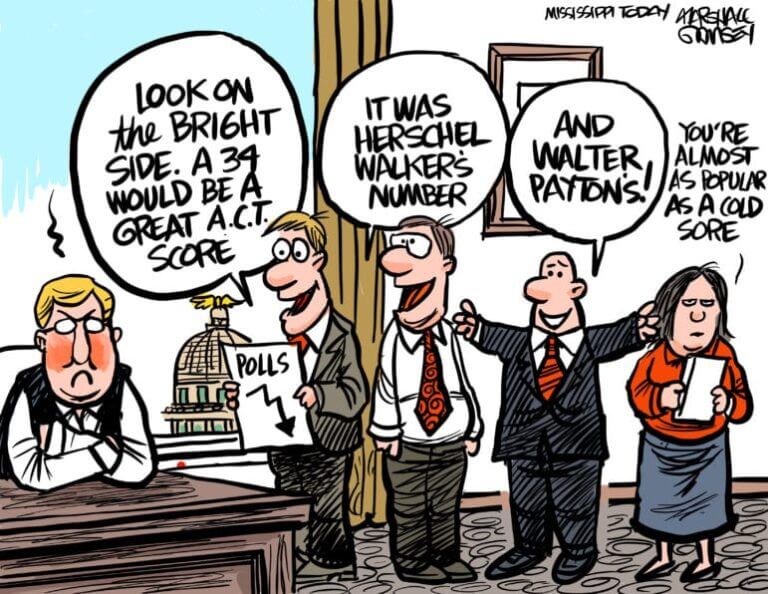
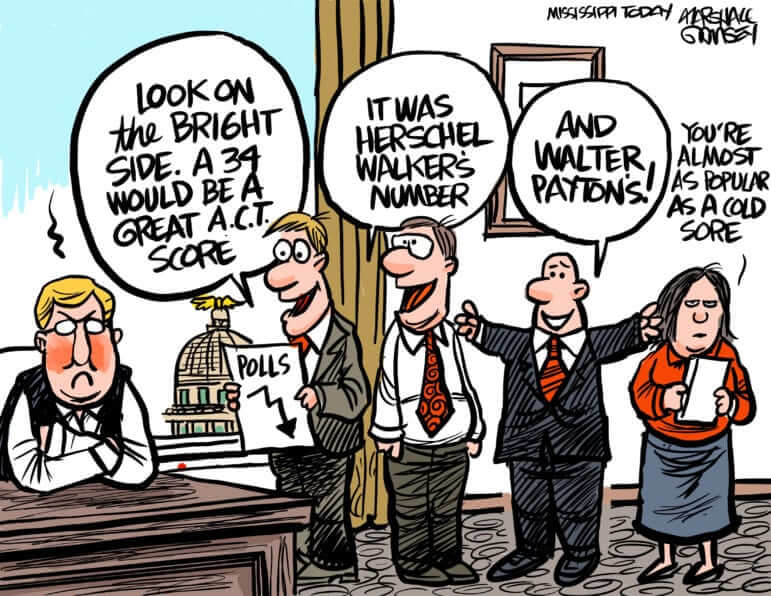
Mississippi elected officials and other politicos responded to the violent outbreak Wednesday afternoon.
- U.S. Sen. Roger Wicker, a Republican, said in a statement: “To everyone who has asked, I am safe. I thank the brave men and women of the U.S. Capitol Police and federal law enforcement for their work to bring this lawlessness and violence in the Capitol building to an end.”
- U.S. Sen. Cindy Hyde-Smith, a Republican, tweeted: “Thank you for the messages of concern. My staff & I are safe. Whatever frustrations any American may have, violence & destruction in the US Capitol, the seat of our democratic government, is unacceptable. I’m grateful for @CapitolPolice & those working to stabilize the situation.”
- U.S. Rep. Bennie Thompson, a Democrat, tweeted: “Locked in Capitol and securing face mask for members… These thugs have no respect for our democracy.”
- U.S. Rep. Steven Palazzo, a Republican, tweeted: “The right to peacefully protest is sacred — and it’s one that must remain protected. Protests must stay peaceful and should not escalate to a point of violence. I am disheartened to see today’s event turn violent and attacked launched against our hardworking police officers. Please pray for this country and the law enforcement officers who are working to keep the peace.”
- U.S. Rep. Trent Kelly, a Republican, tweeted: “Please keep protests peaceful and lawful. I condemn all acts of violence.”
- Republican Gov. Tate Reeves: “Political violence is always wrong. Law and order must win over mob rule. The country we love desperately needs prayer and God’s protection.”
- “I am appalled,” Mike Chaney, the state’s insurance commissioner and Republican Party stalwart, tweeted on Wednesday before quickly deleting the tweet. “A lifelong Republican, one of my worst fears has come true with weak leadership destroying the country and idiots destroying democracy and the Republican Party. Those destroying our Capitol need to be prosecuted!”
- State Rep. Robert Johnson, the House Democratic leader from Natchez, said: “This is a sad day for the country… One person could stop this. I just wish that he would. I am appalled. If it had been a group of African Americans breaking into the Capitol with guns, people would not be standing around watching the Capitol be destroyed.”
- State Rep. Shane Aguirre, a Republican from Tupelo, said: “It is sad to see. Violence and destruction of property is no way to express yourself. I do not condone it in any way.”
-
State Sen. David Blount, a Democrat from Jackson, tweeted: “The logical conclusion to an amoral criminal presidency.”
- Lucien Smith, former chairman of the Mississippi Republican Party, tweeted: “We should all remember opportunists like Senator Hawley, whose dishonest rhetoric contributed to today’s violence, egging on sedition. He and his ilk are not worthy of the offices they hold.”
- Brandon Presley, Democratic public service commissioner: “This scene at the Capitol in Washington is despicable and horrifying. Every American should be praying for the safety all members of Congress and law enforcement. Silence is complicity at this point for anyone who nibbles around the edges. America is NOT governed by mobs.”
- Jason Shelton, Democratic mayor of Tupelo: “Donald Trump’s supporters and a warring foreign nation are the only two groups to ever attack the United States Capitol. Donald Trump is responsible for this and needs to be immediately impeached and removed from office.”
The post Pro-Trump mob storms U.S. Capitol, members of Congress evacuated appeared first on Mississippi Today.